The Epidemic of Non-Alcoholic Fatty Liver Disease
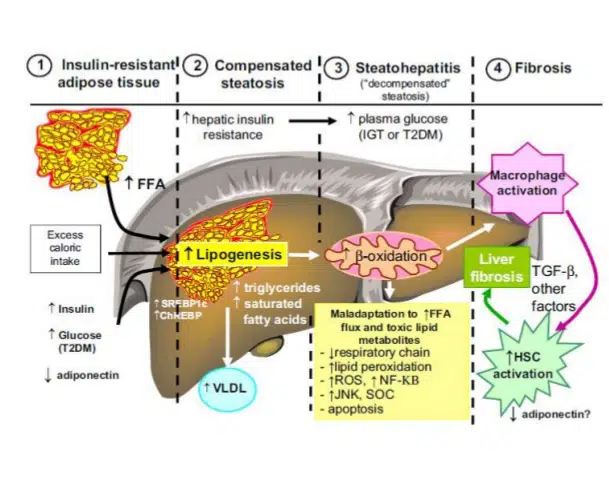
If an individual is obese it is most likely that they suffer from non-alcoholic fatty liver disease or NAFLD. There was a time when this condition was quite rare. Now it appears that more than half of Americans have it and more than a third of American children suffer from it. The condition is generally a function of a diet rich in refined carbohydrates and the concomitant gut problems such as dysbiosis and bacterial overgrowth that feed off the sugar. Together the inflammation and damage to the liver’s detoxification efforts create a significant amount of damage to a person’s health.
There is an enormous amount of protection against NAFLD with a diet high in vegetables and low in sugar. Fiber, mostly fermentable, feeds the right families of beneficial bacteria and is supportive of the intestinal environment that produces less gut wall permeability. This is a critical component of health: intestinal barrier integrity. When an individual is in critical care and requires support via parenteral or enteral nutrition, this topic is essential to understand.
For decades now it has been demonstrated that enteral nutrition is far better, if tolerated of course, than parenteral nutrition. This is mostly because of the influence that available food has on microbial populations within the digestive tract. With something to feed off, microbes can hang around sufficiently enough to generate at least moderate amounts of beneficial substances such as n-butyrate. A recent study showed that parenteral nutrition significantly increases an individual’s risk for NAFLD simply because of the way it undermines the gut-liver axis (1).
Knowing all that we do about the roll of MACs (microbe accessible carbohydrates) found in whole foods as opposed to simple sugars (which get absorbed early in digestion), the potential of enteral nutrition to protect against NAFLD is a function of its wholeness. The supportive qualities of vegetable fiber (fermentable) and specific microbial selective plant-based molecules such as polyphenols and carotenoids, make an enormous difference. These plant-based phytonutrients impart highly beneficial influences on the microbiome, the GI, and subsequently the liver (2).
Too many enteral formulas are centered on sugar, isolated proteins, and seed oils. They provide all of the calories and macronutrients but lack the qualities that are required for good gut health. As a consequence, the liver suffers as well. Studies have shown that a nutrition plan or protocol eliminating fructose and all added sugar can reverse pediatric NAFLD (3). Wouldn’t we want to do the same for children requiring enteral support?
Because so many children and adults suffer with NAFLD and it is driven by inflammation in the digestive tract (4), enteral nutrition needs to evolve to a level beyond calories-protein-RDAs. While this may be considered the foundation of a supportive formula, let’s be clear: fermentable fiber without added sugar is every bit as foundational.
Additionally, while I am at it, please hold the chemicals, preservatives, and emulsifiers like carrageenan. They also cause intestinal inflammation and contribute to the gut wall break down (5). Hopefully the medical community starts to connect the dots with this and other gut-based diseases. Choosing an enteral formula should be an easy decision when these points are considered.
~ John Bagnulo MPH, PhD.
RESOURCES:
1.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5622747/pdf/nutrients-09-00987.pdf
2.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5622722/pdf/nutrients-09-00962.pdf
3. https://www.ncbi.nlm.nih.gov/pubmed/23976771
4. https://www.ncbi.nlm.nih.gov/pubmed/23538296
5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5410598/pdf/fped-05-00096.pdf